Location: Home >> Detail
TOTAL VIEWS
Adv Geriatr Med Res. 2019;1:e190011. https://doi.org/10.20900/agmr20190011
1 Faculty of Physical Activity Sciences, University of Sherbrooke, 2500, boul. de l’Université, Sherbrooke (QC), J1K 2R1, Canada
2 Research Centre on Aging, CIUSSS de l’Estrie-CHUS, 1036, rue Belvédère sud, Sherbrooke (QC), J1H 4C4, Canada
3 Faculty of Medicine and Health Sciences, University of Sherbrooke, 3001, 12e avenue Nord, Sherbrooke (QC), J1H 5N4, Canada
* Correspondence: Eléonor Riesco, Tel.: +1-819-821-8000 (ext. 63337).
Background: Kinesiophobia, the fear that movement and physical activity could worsen side effects such as fatigue and pain, is a barrier to exercise in cancer patients. Physical inactivity and deconditioning can lead to functional decline, higher mortality risk and lower quality of life, in older adults, and even more in oncogeriatrics because of a lower physical activity level during cancer treatments.
The case: We present the case of an older breast cancer patient recruited in a controlled exercise trial and randomized to the control arm of the study (a 12-week supervised static stretching program). She expressed fear that physical activity might exacerbate some of her cancer-related symptoms during baseline physical capacity assessment (Senior Fitness Test, handgrip strength and maximal lower body strength). After completing the 12-week supervised static stretching program, she exhibited similar and/or larger improvements in many of the physical capacity tests than the mixed exercise intervention group, despite being in the control arm.
Conclusions: These observations and physical capacity results have led us to emit the hypothesis that (1) this participant’s baseline physical capacity assessment might have been biased by kinesiophobia and (2) the supervision by exercise physiologist might have mitigated this fear over time. Hence, based on this case, we suggest that kinesiophobia should be measured in future exercise trials and clinical interventions targeting older cancer patients.
CRF, cancer-related fatigue; EX, exercise program; CANEX, cancer-exercise study; FACIT-F, Functional Assessment of Chronic Illness Therapy-Fatigue scale; 1RM, one-repetition maximum; 6MWT, 6-minute walk test; PASE, Physical Activity Scale for the Elderly questionnaire
In cancer patients and survivors, when properly adapted, exercise training is a first line recommendation to reduce cancer-related fatigue (CRF), physical deconditioning, mortality risk and to improve quality of life [1]. This is especially true in older cancer patients, where CRF, physical inactivity and deconditioning are associated with a faster decline in functional capacity, an increased mortality risk and a reduced quality of life, even years after the end of cancer treatments [2–4].
Paradoxically, kinesiophobia, the fear that movement and physical activity could worsen one’s condition, might represent a significant barrier to physical activity in older cancer patients. Kinesiophobia has initially been defined as “an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or reinjury”, leading to avoidance of physical activity, which can result in physical deconditioning, which can, in turn, increase pain and contribute to the loss of functionality [5]. Since the introduction of this initial definition, based on studies in chronic pain patients, this fear-avoidance pattern and subsequent deconditioning has also been described in older adults. The fear of pain have been associated with activity avoidance in this population [6]. The fear of falling has been shown to affect more than 20% of older adults and is one of the main factors explaining activity avoidance [7]. Symptoms of other chronic diseases, like dyspnea in pulmonary diseases [8], and polypharmacy [7] are other factors that have been associated with fear of movement and avoidance in the elderly.
Some data suggest that such fear-avoidance can also represent a barrier to physical activity and exercise in cancer patients and survivors (i.e., having completed cancer treatments). A systematic review of qualitative and quantitative studies identified cancer-related side effects (mainly CRF) and fear of injury as two barriers to physical activity in cancer survivors [9]. Fear that movement could worsen side effects such as pain, CRF and lymphedema has been described as one of the barriers to physical activity in survivors of breast cancer [10], and persistent fatigue in breast cancer survivors has been associated with fear-avoidance beliefs measured by the Tampa Scale of Kinesiophobia-Fatigue [11]. This suggests that all these factors could contribute to kinesiophobia in older cancer patients, but data are missing to truly appreciate how fear of movement could affect participation in physical activity and in clinical exercise programs targeting older cancer patients.
Here, we present the case of an older breast cancer patient allocated to the control arm of a randomized controlled clinical study that sought to evaluate the feasibility and effect of exercise training on CRF and functional capacity in an oncogeriatric population. This participant frequently mentioned her treatment-related side effects (especially pain and occasional dizziness) as well as her fear of movement, and that exercise could worsen her condition. However, these fears seemed to lessen during the supervised static stretching intervention (control group). Furthermore, this participant exhibited surprising post-intervention results considering the absence of proper training.
Altogether, these behaviors and physical capacity results led us to emit the hypothesis that this participant might have presented kinesiophobia at baseline, which could have biased her results during initial physical capacity assessment. Therefore, the purpose of this case study is to address the possible positive effects of exercise supervision on kinesiophobia, and how this could have affected some physical capacity measurements. Furthermore, we aimed to discuss the impact of kinesiophobia on clinical research results. To our knowledge, kinesiophobia has never been considered in clinical exercise trials targeting an oncogeriatric population and is not included in the current clinical exercise guidelines for this population [12].
A 65-year-old woman recently diagnosed with breast cancer was recruited to participate in the CANcer-EXercise (CANEX) pilot study, and randomized in the control arm of the study. Briefly, the CANEX study was a randomized controlled trial aiming to verify the feasibility and efficacy of 12 weeks of supervised, combined exercise (aerobic and resistance training) in older cancer patients undergoing systemic cancer treatments (chemotherapy and hormones therapy). Outcomes measured include CRF (Functional Assessment of Chronic Illness Therapy-Fatigue scale [FACIT-F]) [13] and physical capacity assessment: mobility (six-minute walk test; 6MWT), lower body endurance (30-second chair stand test; CST), dynamic balance (8-Foot Up-&-Go test; 8FUG), upper body endurance (arm curl test; ACT) [14], handgrip strength and maximal lower body strength (Leg-Press 1RM). After medical clearance, all participants were randomly allocated to a mixed exercise program (EX; experimental group) or to a static stretching program (CON; control group). The EX group performed supervised aerobic and resistance exercise training, 2 to 3 times per week. The CON group, in which the present case participant was assigned, performed supervised static stretching 2 times per week, which was used as a «placebo» strategy to reduce dropout rate and control for the impact of exercise specialist supervision. Informed consent was obtained from the participant to have his information published in this case study.
Pre-Intervention MeasurementsDuring the pre-intervention physical capacity testing session, this participant mentioned being preoccupied about side effects associated with her prior chemotherapy treatment (musculoskeletal pain and occasional dizziness episode). These side effects are known to be associated with many chemotherapeutic and supportive drugs [15]. Reassurance was given by explaining the possibility to stop each test upon request, as well as the supervised and progressive and design of the upcoming assessment and intervention, the fact that she had previously obtained medical clearance, and that she could freely resign from the study upon request. She therefore accepted to participate.
Moreover, she mentioned several times that she was afraid to fall or to worsen her symptoms with physical exertion during the tests that involved lower limbs. During the 6MWT, she slowed her walking pace and walked close to the walls on several occasions. She explicitly mentioned that she was uncomfortable with the feeling of exertion, because of previous pain episodes in her ankles following initiation of her chemotherapy treatments. She was also afraid of the possibility of falling. During the 8FUG test, which measures gait speed and dynamic balance, she showed a similar fear of falling, which she also explicitly mentioned. She finally also exhibited a similar fear-avoidance pattern during the leg press 1RM testing procedure, and the test was ended upon her request, leading to a low baseline result at this test (Table 1). She explicitly mentioned after the test cessation that she chose not to “push herself too much”, to avoid exertion, and thus pain exacerbation or injury.
Although to our knowledge there is no specific guideline to diagnose kinesiophobia in cancer patients, such exertion avoidance combined with the fear of falling or worsening of pain have been associated with kinesiophobia in older adults and in patients with chronic pain conditions [7,16]. Thus, these observations led us to suspect kinesiophobia that seemed to be strengthened by the pain and dizziness episodes following chemotherapy treatments reported earlier.
However, it is important to note that this participant did not declare a high level of CRF. Her initial FACIT-F score was 47/52 where a maximal score of 52/52 indicates no CRF, and a threshold score of 34/52 has been proposed as a clinically significant CRF [17]. CRF is the most common side effect in cancer patients, and affects around 80% of all patients [18]. Although kinesiophobia has been associated with a higher level of CRF in cancer patients [10,19], in this case, fear of movement seemed mainly related to symptoms of musculoskeletal pain and sporadic episodes of dizziness in the days following administration of chemotherapy treatments. This is in agreement with the literature having associated pain, fear of falling and side effects of chronic diseases with kinesiophobia in older adults [5,7,16].
The 12-Week Stretching InterventionThe case participant was randomized in the control group and completed a 12-week stretching intervention including 5 to 10 static stretching exercises, twice a week. During the first month of the intervention, the participant exhibited additional patterns of kinesiophobia. She reiterated her fear that stretching could exacerbate pain or other cancer-related symptoms, as well as her fear of falling. Whenever required, reassurance was given by the exercise physiologists supervising the intervention.
Interestingly, as the intervention progressed, accumulating signals led the team to suspect that her initial fear of movement and exertion was gradually decreasing: The participant mentioned several times that she was less afraid about exercise in the second half of the intervention. Her husband also mentioned that she was more confident in her activities of daily living.
During the last month of intervention, the participant mentioned twice that she wished to begin aerobic exercise training. To avoid any bias in the clinical randomized exercise trial, she was invited to wait upon the end of the 12-week stretching program.
Post-Intervention MeasurementsDuring the post-intervention evaluation, the case participant clearly showed signs of reduced fear of movement and mentioned that she found the assessment less frightening than at baseline.
Of note, considering the three tests where the participant expressed fear of falling or worsening her symptoms at baseline (6MWT, 8FUG, 1RM leg press), her baseline results were under the lower bound of the 95% confidence interval (CI) of the rest of the overall sample (Table 1). From a clinical standpoint, her pre-intervention results could be considered low with the 6MWT distance and the 8FUG time under the 25th percentile [14], as well as the leg press 1RM under the 10th percentile [12].
However, the post-intervention changes (post- minus pre-intervention result) of the case participant at these tests were comparable to the improvement of both groups, except for the 8FUG, where her improvement was higher than the 95% CI of both groups.
Such improvements seemed surprising, as this participant neither underwent aerobic nor resistance exercise training and did not increase her total physical activity level aside from the stretching intervention (as confirmed by the Physical Activity Scale for the Elderly (PASE) questionnaire [20], used to assess pre- and post-intervention total physical activity level as a control variable). The improvement observed to the 8FUG test is particularly striking as it resulted in a change from the 25th percentile to almost the 75th percentile based on the reference values proposed for the Senior Fitness Test Battery for a 65–69 years old woman [14] (Figure 1).
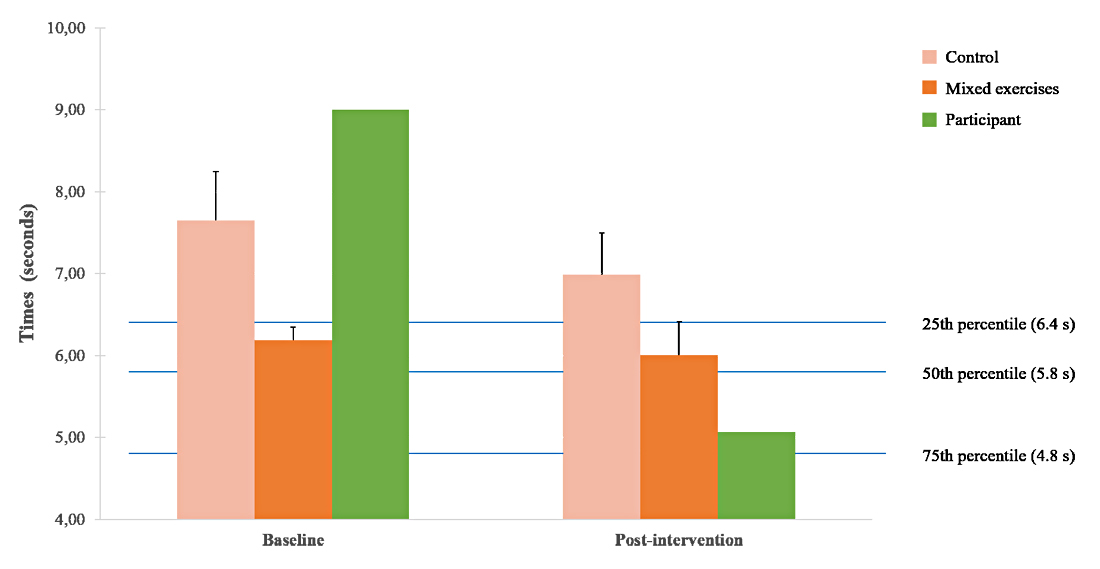 Figure 1. Pre-post intervention difference for dynamic balance (8FUG). Group results are presented as mean ± standard error of the mean. The 25th, 50th, and 75th percentiles represented are the values proposed by Rikli & Jones (1999) [14] for 65 to 69-year-old women.
Figure 1. Pre-post intervention difference for dynamic balance (8FUG). Group results are presented as mean ± standard error of the mean. The 25th, 50th, and 75th percentiles represented are the values proposed by Rikli & Jones (1999) [14] for 65 to 69-year-old women.
Many indicators of this participant’s perception towards exercise suggest that she was struggling with kinesiophobia when she initiated the CANEX pilot study. The case participant extensively expressed her fear about exertion and symptoms exacerbation prior to and during the intervention. Nevertheless, these fear and avoidance patterns seemed to have lowered during the 12-week supervised stretching intervention. Three hypotheses can be drawn from this case and will be discussed further in the following sections.
Kinesiophobia Might Represent a Bias in Physical Capacity Testing in Trials and Clinical PracticeThere are some evidence supporting the idea that kinesiophobia might represent a potential confounding factor in physical capacity assessment in older adults. Associations have been found between kinesiophobia measured with the Tampa scale and physical capacity tests assessing gait speed and dynamic balance. In older women with chronic musculoskeletal pain, an association was found between the Tampa scale score and the result for the Timed up-and-go test (almost identical to the 8FUG test) [16,21]. Similarly, an association was found in older adults with COPD between symptoms-related kinesiophobia and poorer results to the 6MWT [22].
To our knowledge, to date, no study has investigated if such an association exist between kinesiophobia in older cancer patients and lower scores in gait speed and balance measurements. In this context, the present case led us to suspect that this participant’s initial fear and avoidance of exertion could have biased to a certain extend the initial results of her physical capacity measurements, thus not entirely reflecting a true improvement in physical capacity at post-intervention. As stated above, the case individual presented here clearly mentioned that she preferred walking slower because of her fear of falling while performing the 8FUG test and the 6MWT at baseline and mentioned being less afraid during post-intervention evaluation. Therefore, we hypothesized that kinesiophobia might, at least partly, represent a confounding factor during physical capacity assessments in oncogeriatrics.
It is important to note that other factors may also have contributed to the observed changes, such as the learning effect. Nevertheless, as no pre-testing were performed, it can be hypothesized that all participants may have equally benefit from such an effect. Moreover, the fact that baseline assessment took place four days after chemotherapy administration could have also resulted in residual treatment side effects that could have also partly affected her results. However, for every participant of the study, post-intervention testing was performed according to the same treatment calendar (i.e., the delay between baseline assessment and the last chemotherapy treatment administered was reproduced for post-intervention assessment to minimize the potential confounding effect when analyzing pre-post changes).
Possible Positive Impact of Exercise Supervision on Kinesiophobia and Exercise ParticipationDespite clearly showing fear of physical exertion at baseline, the case participant freely chose to participate in the exercise trial and completed the 12-week stretching intervention. Interestingly, the results of a qualitative study in cancer survivors mentioned that the lack of knowledge about exercise and the fear of worsening their condition were major barriers to exercise participation, and that supervision by exercise specialists would be a determining factor in deciding to engage in regular exercise [9]. Moreover, supervised exercise combined with kinesiophobia management was shown to result in lower disability scores than exercise alone in a rehabilitation program for chronic pain conditions [23].
This led us to hypothesize that exercise supervision and reassurance given by the exercise physiologists could have influenced positively her choice to participate and remain in the study. Unfortunately, to our knowledge, no quantitative or qualitative studies so far have assessed the effect of exercise supervision on kinesiophobia in oncogeriatrics, or even in older adults without a cancer history. Therefore, we suggest that future studies should verify the effect of exercise supervision on fear and avoidance of movement in older cancer patients.
Kinesiophobia in Older Cancer Patients Might Not Always Be Explained by Cancer-Related FatigueFinally, it appears important to note that, to our knowledge, the only studies concerning cancer symptoms-associated kinesiophobia have focused mainly on CRF [10,11]. In a validation study, Velthuis et al. [11] showed that the Modified-Tampa Scale of Kinesiophobia-Fatigue (initially developed in chronic fatigue syndrome patients) is associated with CRF measured by the FACT-F questionnaire. Hence, so far, the only validated tool to measure kinesiophobia in cancer patient is the Modified-Tampa Scale of Kinesiophobia-Fatigue, designed only with questions targeting fatigue-related kinesiophobia.
However, this case individual did not exhibit CRF neither at baseline nor post-intervention, according to her FACT-F scores. Moreover, no difference was found between this participant and each group at both time points of the study. She rather mentioned that her fear of exertion was related to episodes of pain and dizziness following chemotherapy treatment.
Although it remains impossible to draw conclusions from this single case, it is known that other factors aside from fatigue can be associated with kinesiophobia in older adults, such as a lower perceived physical capacity, the fear of falling or pain [6–8]. This led us to hypothesize that the Modified-Tampa Scale of Kinesiophobia-Fatigue might not be sufficient to assess kinesiophobia in older cancer patients, therefore underestimating the prevalence of kinesiophobia in this population.
Nevertheless, Verwoerd and colleagues [24] showed that, in low back pain patients, asking to rate on a 0–10 scale their fear that physical activity could increase their symptoms was a valid method to quickly assess kinesiophobia. We thus suggest that validating this simple tool in older cancer patients could represent a practical way to measure kinesiophobia in this population.
Some evidence support the ideas that kinesiophobia could interfere with physical capacity measurements [16,21,22] and that professional exercise supervision and kinesiophobia management might have a positive effect in exercise adherence in chronic pain conditions [23]. The present case participant led us to hypothesize that this could also be the case in older cancer patients. This is an important issue, considering the negative effects of deconditioning and inactivity on physical function and quality of life in older cancer patients and survivors [2–4].
Nevertheless, we acknowledge that cautiousness must be kept in mind when discussing the results of this case individual in comparison to the overall study sample. These reflections remain hypotheses based on a case study since it was not initially intended to measure kinesiophobia. To our knowledge, no clinical exercise study targeting an oncogeriatric population included such a measurement so far. Therefore, from a research perspective, we believe that kinesiophobia should be measured in future exercise trials, to verify if it really has an impact on physical capacity outcomes, and if exercise supervision by specialists could affect its evolution during a training intervention. We suggest that future exercise trials in older cancer patients and survivors should include the Modified-Tampa Scale of Kinesiophobia-Fatigue [11] combined with a 0–10 Visual Analogue Scale including frequent cancer-related symptoms such as pain.
Finally, from a practical perspective, this case study also suggests that exercise specialists should pro-actively assess and monitor kinesiophobia in older cancer patients and survivors and consider kinesiophobia in their exercise testing assessments and prescription. Considering the impact of kinesiophobia in adherence to physical activity in older adults [6,7], and the demonstrated impacts of kinesiophobia management during exercise supervision programs in other conditions such as chronic pain [23], it could have major effects on long-term physical activity level and associated-benefits.
The dataset of the study is available from the authors upon reasonable request.
MP, ER and TF designed the study, and AF and HPR designed the exercise training interventions. AF, RM and HPR administered the testing and measurements and supervised the training and stretching interventions. RM and HPR analyzed the data and wrote the manuscript, and IJD, AF, TF, MP and ER reviewed it.
The authors declare that they have no conflicts of interest.
The study was funded by the Faculty of Medicine and Health Sciences, Université de Sherbrooke.
The authors gratefully thank all participants of the CANEX study.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
Parent-Roberge H, Maréchal R, Fontvieille A, Dionne IJ, Fülöp T, Pavic M, et al. Breaking Barriers: Could Have Exercise Supervision Attenuated Kinesiophobia in an Older Cancer Patient? Adv Geriatr Med Res. 2019;1:e190011. https://doi.org/10.20900/agmr20190011

Copyright © 2020 Hapres Co., Ltd. Privacy Policy | Terms and Conditions