Location: Home >> Detail
TOTAL VIEWS
Adv Geriatr Med Res. 2025;7(3):e250020. https://doi.org/10.20900/agmr20250020
1 Faculty of Arts and Humanities, Universidade da Madeira, Madeira 9020-105, Portugal
2 2256c Health, Ltd., Lisboa 1269-039, Portugal
* Correspondence: Luísa Soares
Stroke is one of the leading causes of death worldwide, with consequences that impact physical, mental and emotional health, and social life of survivors. Social support is fundamental to promote rehabilitation and quality of life of stroke survivors. Objective: investigate the impact of therapeutic groups in promoting social support and well-being among stroke survivors, as well as to understand how therapeutic writing, mediated by WhatsApp, can contribute to strengthening group dynamics. Methods: a systematic literature review in different databases, on B-on, Pubmed, and Google Scholar. Results: therapeutic groups are crucial in improving quality of life and providing emotional support, self-reflection, and interpersonal relationships. Digital technologies, such as WhatsApp, are effective in facilitating communication and mitigating social isolation, benefiting survivors and their caregivers. At the same time, Therapeutic Writing has proven to be a valuable strategy for emotional expression, contributing to resilience and intragroup cohesion. Conclusion: Integrating digital technologies in rehabilitation is promising, offering new possibilities for inclusive and effective interventions. Innovative and multidisciplinary approaches that use accessible technologies and maximize the support and well-being of stroke survivors and caregivers are one of the avenues for future research.
Stroke remains a leading cause of death and the primary cause of disability worldwide [1]. Over the past 17 years, lifetime stroke risk has increased by 50%, with 1 in 4 people expected to experience a stroke [2]. In Portugal (2022), stroke caused 9616 deaths—7.7% of all mortality—with a rate of 92.1 deaths per 100,000 people. Women were more affected, though they died later than men on average (83.9 vs. 79.8 years) [3]. In Madeira, 184 cerebrovascular deaths occurred in 2021, mainly in Funchal [4]. Projections suggest stroke-related deaths will rise 45% by 2035, with lasting effects increasing by 25% [5,6].
Improved acute care has increased survival rates [7], but stroke’s chronic effects impact physical, mental, and emotional well-being [8–10], often resulting in cognitive, social, psychological, and functional challenges [7–11]. Symptoms may include memory and speech issues, fatigue [12,13], and emotional disorders like depression and anxiety [9,11], exacerbated by lifestyle disruptions and reduced social interaction [10]. About one-third of survivors develop post-stroke depression, impeding rehabilitation [14]. They may feel worthless, hopeless, or burdensome [9,11], with fears about the future and daily functioning [11].
Emotional, cognitive, and physical changes—alongside shifting family and social roles—may alter survivors’ identities [11]. Communication problems, mobility issues, and job loss can lead to social isolation and stigma, often worsened by socioeconomic factors [11,15]. Yet, personal resilience and community support are key for reintegration [15]. Support from family, community, and healthcare professionals—including psychologists—is essential for managing emotional health and recovery [15,16].
Caregivers share these challenges. Around 80% of stroke survivors return home, with half requiring ongoing care, typically from family [7,17,18]. This role demands emotional and physical labor, increasing stress and risk of burnout [17,18]. Caregiving affects well-being, lifestyle, and caregiving effectiveness [7,18]. Thus, caregivers need support to maintain their health and improve quality of life for both parties [7,16]. Educational programs can improve caregiver knowledge, reduce delays in care, and foster patient independence [17].
Technological Tools: Mobile Apps & WhatsAppThe rise of mobile communication apps like WhatsApp and Instagram has made text messaging a primary form of contact [19,20]. More than a convenience, text messaging is now a widely accepted tool in digital therapy. The growth of e-therapy—fueled by tech advances and the COVID-19 pandemic—has expanded therapeutic formats to include real-time text communication [20,21]. WhatsApp enables personalized, portable, and accessible communication, offering users control over how and when they express themselves [20].
Text-based therapy has several advantages: it enhances intimacy and trust, fosters self-reflection, and can better suit personal disclosure than face-to-face settings [20,23]. The visual style of texts may even reflect emotional states, and stored messages provide valuable material for therapeutic review [23]. Texting, alone or with in-person therapy, is a flexible and effective approach.
Text message interventions have shown positive behavior changes across demographics, even without high personalization [23]. WhatsApp, launched in 2010, is widely used for its ease and versatility—supporting video calls, image sharing, emojis, and real-time interaction [24–26]. It's already used in clinical settings to form support and rehab groups [24], proving effective in diverse populations: from smoking cessation to autism support [27], domestic violence victims [28,29], and recently, stroke survivors [10]. Reported benefits include social support, therapy adherence, increased life satisfaction, emotional help, and peer exchange of coping strategies [19,26–30].
Therapeutic Writing & WhatsApp IntegrationTherapeutic Writing involves expressing thoughts and emotions through writing to enhance self-awareness, insight, and well-being [31–33]. It helps individuals process mental health issues like anxiety and depression [31], facilitating emotional regulation and meaning-making through narrative creation [31,33].
The integration of technology has influenced Therapeutic Writing practices, with online formats emerging as innovative therapeutic options [32]. Writing fosters cognitive clarity and emotional expression, making it a versatile tool in mental health interventions [33].
For the purposes of this review, ‘therapeutic groups’ were defined as structured, facilitator-led sessions involving two or more participants, designed to achieve specific therapeutic objectives (e.g., emotional processing, cognitive restructuring, or peer support) and guided by an established therapeutic framework (such as CBT, psychodynamic, or expressive therapies). ‘Therapeutic writing interventions’ were defined as structured writing activities with explicit therapeutic intent, including reflective journaling, expressive writing, or narrative therapy tasks, delivered in individual or group formats. Both face-to-face and digital delivery modes were considered, with WhatsApp-mediated interventions being one of several possible modalities. Studies were included if they met these criteria, regardless of setting, provided the intervention was delivered by or under the supervision of a trained facilitator or therapist.
Study FocusThis systematic review explores how therapeutic groups promote social support and well-being among stroke survivors, emphasizing the role of therapeutic writing and WhatsApp. WhatsApp’s real-time interaction can strengthen group communication and offer consistent support. The study examines not only the emotional and social benefits of group therapy but also how mobile technologies enhance group cohesion and survivor well-being.
Social support’ was defined as the perception or experience of being cared for, valued, and part of a reciprocal social network. Where applicable, we distinguished between perceived social support and received social support. Operationalization in the included studies was based on validated instruments such as the Multidimensional Scale of Perceived Social Support (MSPSS), the Social Support Questionnaire (SSQ), or comparable tools.
‘Well-being’ was conceptualized in accordance with two dimensions: hedonic well-being (e.g., life satisfaction, positive affect) and eudaimonic well-being (e.g., sense of purpose, personal growth). Measurement tools included, for example, the WHO-5 Well-Being Index, Ryff’s Psychological Well-Being Scales, or equivalent validated measures. This classification allowed for a consistent approach to data synthesis while respecting the conceptual frameworks.
A Systematic Literature Review is a research method that synthesizes existing literature using defined protocols for search, analysis, and integration, providing coherence and meaning to a body of evidence on a specific topic [34,35].
ObjectivesThis review aimed to:
(a) Explore the impact of therapeutic groups on social support and well-being of stroke survivors, focusing on emotional and social benefits;
(b) Analyze how WhatsApp can mediate interaction, strengthen group bonds, and expand support through therapeutic writing.
Research Questions1.
2.
3.
4.
The review followed PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [36].
Research StrategyThe search protocol used combinations of the following terms:
●
●
●
●
●
Boolean operators (AND, OR) and truncators (“*”, “”) ensured inclusiveness.
Searches were conducted in PubMed, B-On, Google Scholar, and Google, in English and Portuguese, covering the period 2000–2025. Filters in the B-On database aligned with the inclusion/exclusion criteria. Keyword searches were applied to article titles and content. The B-On search initially yielded 1863 results.
Although Google is not a primary scientific literature database, it was included as a supplementary search tool to identify grey literature and potentially relevant materials not indexed in traditional databases (theses, institutional reports, and documents from professional organizations). This approach aimed to minimize publication bias by capturing evidence that might otherwise be excluded from the synthesis. The use of Google was conducted in a structured manner, with predefined keywords and search limits to reduce selection bias and maintain methodological rigor.
Inclusion Criteria●
●
●
●
●
●
●
●
Studies were excluded as ‘irrelevant to the research questions’ if they met one or more of the following conditions: (1) the intervention described was not therapeutic in nature (e.g., purely informational or educational programs without a therapeutic component); (2) the primary outcomes did not include social support, well-being, or closely related constructs; (3) the population studied did not match the target group (e.g., different age range, clinical condition, or setting); (4) the study focused exclusively on technology development or platform usability without assessing therapeutic impact. These specifications ensured consistent and transparent application of the exclusion criterion during the screening process.
The search was conducted between 15 of September till 31st of December 2024. A PRISMA flowchart (Figure 1) outlines the selection process, including duplicate removal and full-text assessment. For each eligible study, author, year, title, journal, and key conclusions were extracted and presented in Results Analysis Tables.
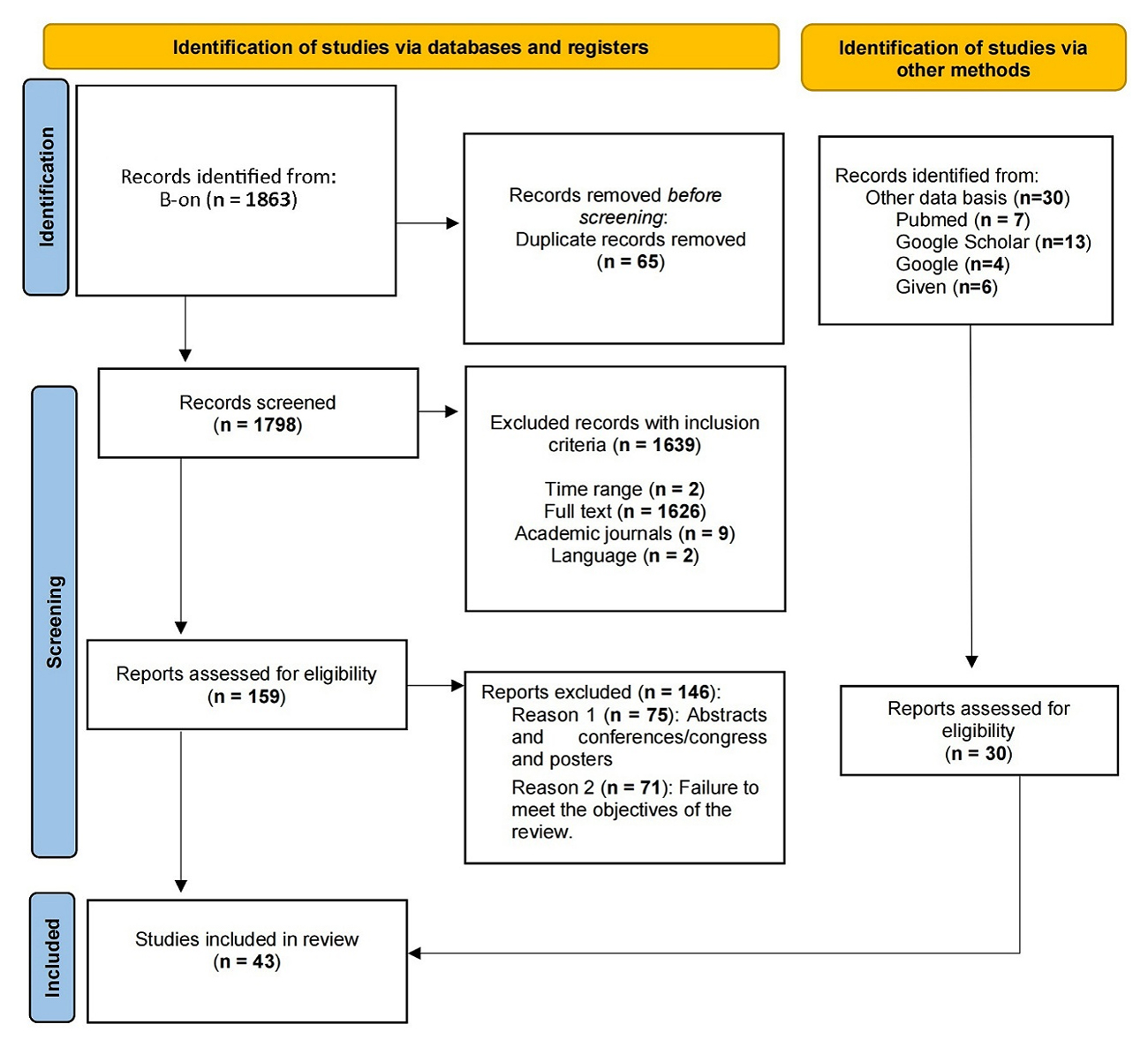 Figure 1. PRISMA 2020 [36].
Figure 1. PRISMA 2020 [36].
The methodological quality and risk of bias of the included studies were systematically assessed according to their study design. For randomized controlled trials (RCTs), the Cochrane Risk of Bias tool (RoB 2.0) (Cochrane Collaboration, London, UK) was used, evaluating domains such as randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results.
For non-randomized quantitative studies, the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS) was applied, assessing selection of participants, confounding variables, measurement of exposure and outcomes, blinding, incomplete outcome data, and selective reporting.
For qualitative studies, an appropriate quality appraisal tool (e.g., CASP checklist) was used, focusing on study design, recruitment strategy, data collection, analysis, and researcher reflexivity.
All records retrieved through the systematic search were screened independently by two reviewers based on titles and abstracts. Full-text articles deemed potentially relevant were then independently assessed by the same two reviewers against the predefined eligibility criteria.
Data extraction from included studies was also performed independently by two reviewers using a standardized data extraction form, which captured information on study design, participants, interventions, outcomes, and results. Any disagreements during study selection or data extraction were resolved through discussion between the two reviewers. If consensus could not be reached, a third reviewer was consulted to make the final decision.
This process ensured consistency, minimized errors, and reduced potential selection bias, in line with PRISMA 2020 recommendations.
Data SynthesisThe findings from the included studies were synthesized using an arrative and thematic approach, rather than relying solely on tabular presentation. Studies were grouped according to key outcomes, such as social support and well-being, and according to the type of intervention (e.g., therapeutic writing, group therapy, digital interventions).
Within each group, patterns, similarities, and differences among studies were systematically analyzed. Particular attention was paid to the study design, sample size, methodological quality, and risk of bias, to contextualize the strength and reliability of the evidence.
The narrative synthesis highlights trends, key findings, and gaps in the literature, while tables are used as complementary tools to summarize study characteristics, interventions, and outcomes for easier reference.
This combined approach ensures a rigorous and transparent synthesis of evidence, facilitating a comprehensive interpretation of results in line with PRISMA 2020 guidelines.
Due to the substantial heterogeneity among the included studies, including differences in interventions (e.g., WhatsApp-mediated vs. other digital support), outcomes (various measures of social support and well-being), study designs, and follow-up durations, a meta-analysis or pooled effect size estimation was not feasible without risking misleading conclusions.
Therefore, a structured narrative synthesis was employed. This approach allowed for systematic summarization and critical appraisal of the evidence, considering study quality, sample size, outcome variability, and risk of bias.
While narrative synthesis does not provide quantitative effect, it enables transparent reporting of patterns, trends, and gaps in the literature, and facilitates discussion of heterogeneity, limitations, and implications for future research.
The search identified 1863 studies. The selection criteria applied resulted in 224 articles for analysis. After removing duplicate articles, 159 studies proceeded to initial screening. The titles and abstracts were analyzed, resulting in the exclusion of studies, mainly for two main reasons:
1. compiled conference or congress papers, and posters were not intended for analysis (n = 75).
2. Studies that did not address the intended theme. Many articles have emerged related to topics about children with leukaemia and their caregivers; about COVID-19 in general, not specified for the stroke survivor population; about hip fracture; about bipolar disorder and autism spectrum disorder; about musical groups, about heart failure, which resulted in the exclusion of 63 articles.
From this initial stage, only 21 articles were submitted for full-text verification.
As a result, 13 studies met the inclusion criteria and were analyzed. As it is a relatively recent topic, the total number of studies found through the research protocol and effectively submitted for analysis for this review was insufficient. Thus, 30 articles were added to this review to complement the intended information and objectives.
The included studies were considered mixed studies and their details such as specific population, sample size, detailed intervention, key outcomes and their measurements were presented wether in the colune of the main conclusions.
Results Analysis 1: Stroke Survivors and CaregiversIn Table 1, we observe that stroke survivors experience sudden, life-altering changes that demand personal and family adaptations [37]. These changes involve complex care needs—physical, psychological, social, and environmental—placing significant strain on families [38]. Understanding family dynamics is crucial, as caregiving typically falls on them. The emotional, physical, and financial pressures can destabilize family life and elevate stress levels [37]. Family caregivers play a central role but often face challenges that affect their well-being, highlighting the need for supportive interventions for both caregivers and survivors [37].
Medical advances have improved acute stroke treatment, increasing survival rates. However, this has led to more individuals living with long-term complications, particularly cognitive and emotional issues during the chronic phase [39]. Therefore, accessible, low-cost strategies are needed to slow cognitive decline and prevent neurodegeneration [39]. Despite progress in medical care, recovery still heavily depends on rehabilitation [40]. Effective recovery requires integrating physical rehabilitation with cognitive and emotional activities, within a structured, supportive group setting [38].
Many families struggle to adapt in the first six months post-stroke. Targeted support during this critical period is essential to enhance social support, reduce caregiver burden, and restore family functioning [37].
Results Analysis 2: Therapeutic WritingWriting has long complemented psychotherapy across different approaches [41,42]. James Pennebaker introduced the Expressive Writing Paradigm, where participants wrote about traumatic experiences for four days, showing that writing helps those facing deeply personal traumas [43,44] (see Table 2). This process fosters emotional expression, improves physical and mental health, and encourages adaptive behaviors by promoting reflection and emotional regulation [42,45].
Writing enables individuals to explore significant experiences freely, aiding cognitive organization, social integration, and communication. Research shows that constructing personal narratives improves mental and physical health across diverse populations, regardless of age, gender, or background [42,46]. Compared to writing about neutral topics, expressive writing has been linked to fewer medical visits, stronger immune function, and reduced emotional suffering [43,46].
Its benefits include:
(a)
(b)
(c)
(d)
Health benefits depend on translating emotions into language, reshaping how individuals understand trauma. Narratives connect causes and consequences, helping individuals make sense of their experiences, boosting well-being [43,46].
Writing also strengthens social bonds by encouraging emotional sharing and memory-building [33,44]. The more intense the emotion, the stronger the desire to share. This fulfills both personal reflection and social connection. Expressive writing influences everyday behavior and language, reinforces therapeutic relationships, and fosters validation and emotional support [42,44].
In online interventions, combining Expressive and Positive Writing paradigms has shown promise. Motivation for change enhances effectiveness by reducing rumination and stress [47]. Balancing these writing styles aligns with individual cognitive styles and supports coping with life’s challenges [47].
Batista J, et al., 2022 [48] introduced the concept of Moments of Innovation (MI) in therapy—key shifts in a client’s discourse that signal emotional or cognitive breakthroughs. Though typically used in psychotherapy, they offer insights into broader processes of personal transformation.
Expressive writing is cost-effective, rapid, and suitable for various populations [45,47]. It has proven beneficial in managing health challenges, including complex grief. For example, it supports grieving mothers after early pregnancy loss and palliative care patients, improving quality of life for both patients and healthcare providers [49–51].
Stroke, seen as emotional trauma due to its sudden onset and lasting impact, can benefit from writing as therapy [41]. Writing during recovery—such as using diaries—helps stroke survivors and caregivers manage fatigue, plan routines, and identify triggers [13]. It supports coping, enhances awareness, and strengthens retrospective understanding of daily life.
Group narrative writing post-stroke promotes belonging and accomplishment. Finding safe spaces for emotional sharing remains therapeutic even years into recovery [41]. Writing supports emotional regulation, social connection, and acceptance of past events while helping individuals make decisions and set goals [41,42]. The act of writing—by hand or digitally—can also promote mindfulness and relaxation.
Survivors have used vlogging similarly to journaling, tracking recovery and building community, while caregivers use social media to express challenges, highlighting its value as a support and communication platform [1].
Results Analysis 3: Therapeutic GroupsIn Portugal, GAMs, i.e., Mutual Aid Groups, formed as a priority initiative of Portugal AVC Association, following the examples of England and United States (see Table 3). These groups aim to encourage stroke survivors to share their experiences related to health problems and/or to face limitations in their motor, communicative, sensory, cognitive, or other capacities resulting from the stroke [52].
They function as a space for inclusive dialogue between peers, which can contribute to mitigate difficulties faced by participants and foster positive changes on a personal and/or social level. They aim to reduce the social isolation experienced by people who directly experienced the event and their family members and caregivers. In addition to stroke survivors, their family members, caregivers, and health professionals, e.g., can participate [52]. Joining therapeutic groups to discuss trauma can be beneficial as interactions bring a new perspective and validate experiences [41].
GAMs offer several benefits. For survivors, therapeutic groups promote self-esteem, personal growth, and help face both physical and psychological challenges. They reduce isolation, increase disease knowledge, and support recovery. These groups help develop coping skills for limitations at individual, family, and social levels. Feeling a sense of belonging—through public, corporate, or media engagement—raises awareness of patient rights and specific needs [52].
Peer support groups are vital for psychological adjustment after a stroke [16]. They provide a space to share experiences, manage long and uncertain rehabilitation, and recognize shared struggles like loss, loneliness [11,15,41], depression, anxiety [6], and uncertainty. They encourage celebrating small victories and maintaining hope. Members support each other, emphasizing independence and control over their lives [6,41].
Participants valued group interaction, bonding, and expressed gratitude [41]. Peer groups and conversations with others at a similar recovery stage offer meaningful psychological support [13,16].
Survivor groups and support systems play a key role in emotional support and community involvement, both essential for recovery [10]. They also promote health literacy and psychoeducation for survivors and caregivers regarding prevention, condition management, and adherence to therapy [6].
Support communities provide emotional, social, and practical help, easing the challenges of the condition and improving well-being [10]. They also benefit caregivers by offering coping strategies and shared responsibility. By creating a safe space for emotional expression and empathy, these groups enhance quality of life, especially where resources are limited [6]. They are also a cost-effective complement to formal mental health services, addressing psychological and social needs more accessibly and easing pressure on health systems [6].
Results Analysis 4: Technological Advances, Mobile Applications—WhatsApp and Therapeutic GroupsThe World Health Organization defines e-health as the use of Information and Communication Technologies (ICT) in healthcare—a rapidly growing field [53]. E-health enables cost-effective, secure healthcare services, including monitoring, education, and research (see Table 4). It enhances global healthcare delivery and makes systems more responsive to patients’ needs [54].
To reach and support stroke survivors, innovative methods like e-health are vital. Technology offers numerous possibilities for stroke treatment, prevention, and education, especially through the Internet for those with disabilities [55]. Stroke survivors, at high risk of recurrence, need ongoing support and education [55]. Rehabilitation is central to recovery, but adherence is often challenging due to symptoms [56]. As it demands significant time and resources, efficient delivery of rehabilitation services is critical [57].
Social media has shown potential for ethically supporting stroke patients, particularly during COVID-19, when it became essential for information sharing, patient support, and rehabilitation [1]. The pandemic worsened isolation and mental health across society, with stroke survivors—already vulnerable—experiencing even greater challenges [22,58]. Many reported disrupted routines, reduced face-to-face interactions, and increased reliance on technology to stay connected [22]. This highlighted the need for strategies that promote emotional well-being, digital inclusion, and virtual programs to combat isolation [22].
The pandemic accelerated the use of technology across health and rehabilitation. [59] explored how stroke group members maintained connections and psychosocial well-being during social isolation. Though in-person meetings stopped, groups adapted by communicating through letters, phone calls, emails, text messages, video calls, and platforms like WhatsApp, Zoom, and Facebook [59]. These tools preserved social support and a sense of belonging, crucial for reducing loneliness, boosting self-esteem, and improving well-being [59]. While online formats pose challenges, strong relationships can be sustained with deliberate effort, making virtual therapeutic groups an effective tool for meeting psychosocial needs [59].
Zhang W, et al., 2023, [38] demonstrated the success of online clinical trials among stroke survivors, particularly in the MindFit project. This randomized study compared the effects of combined therapies—Mindfulness-Based Stress Reduction (MBSR), physical activity, and Computerized Cognitive Training—on emotional and cognitive outcomes. Participants, grouped by intervention via WhatsApp, reported that MBSR improved emotional regulation, self-awareness, stress, pain management, and acceptance of life post-stroke.
The online format was widely appreciated for its accessibility and flexibility, especially for individuals with mobility issues or in remote areas [38]. It also offered psychological safety by reducing physical exposure, which helped decrease stigma and increase comfort during participation. This welcoming environment encouraged engagement, particularly for those vulnerable to face-to-face settings. The group format was a key element, offering emotional support, motivation, and a space to share challenges and progress, strengthening participants’ sense of community [6,13,38].
Lamont RA, et al., 2022, [60] explored compassion in virtual peer support programs for stroke survivors, emphasizing their effectiveness. Compassion emerged through facilitators’ qualities—empathy, genuineness, dedication—and through virtual strategies such as warm tones, positive facial expressions, camera eye contact, emojis, and “virtual hugs.” Despite the absence of physical presence, the virtual format enhanced accessibility and inclusion. Success depended on facilitators’ ability to personalize interactions, adapt communication (e.g., for aphasia), and foster a safe digital environment [60].
In recent years, digital health technologies have proven valuable in supporting stroke survivors, especially through mobile apps [1]. Social media enables content creation, engagement, education, and outreach to survivors, caregivers, and professionals. Platforms like WhatsApp are intuitive, practical, and widely accessible, supporting varied communication needs [1].
Studies show WhatsApp promotes long-term, at-home rehabilitation engagement [10,56]. Clancy B, et al., 2022, [56] highlighted the ability of physiotherapists to tailor strategies based on individual needs, stroke severity, and available support. Therapist availability for feedback and encouragement improved patient accountability and motivation.
Esther CO-W, et al., 2013, [10] showed WhatsApp facilitated real-time emotional sharing, strengthened group bonds, and provided consistent peer support—something limited by infrequent in-person meetings. Its familiar interface made participation accessible and continuous, complementing face-to-face sessions.
WhatsApp also supports supervision, feedback, and discussion—individually or in groups—through text, audio, and video. Sharing pre-recorded content and tracking clinical outcomes reinforced social engagement and built self-confidence through recognition of progress [1,56]. Harrison M, et al., 2017, [17] found that adding caregivers to WhatsApp groups helped clarify doubts about daily care routines and exercises.
Reminder messages sent via WhatsApp played a critical role in keeping participants engaged, aligned with goals, and aware of their rehabilitation progress [10,56]. These interventions reinforced activity adherence and supported emotional well-being.
Social media is increasingly integral to stroke care, marking a paradigm shift [1]. It reconnects survivors with broader communities, facilitating progressive reintegration. As a communication tool, WhatsApp effectively disseminates health information and improves access to services, offering practical, fast, and inclusive support [61].
While traditional in-person groups support emotional health and social networks, integrating digital tools enhances reach and flexibility. Hybrid models—blending face-to-face and online interactions—sustain peer connection, foster emotional sharing, and create more inclusive, accessible, and cohesive support environments [10].
Integrating digital technologies into support groups significantly enhances communication, self-reflection, and group interaction [38]. Tools like the “Queijinho” feedback model [10] foster emotional awareness and strengthen community bonds, contributing to sustainable collective emotional health. By eliminating geographical and mobility barriers, virtual formats improve accessibility and inclusivity, making rehabilitation strategies more effective [38].
Participation in virtual groups builds resilience against isolation, reinforcing the need to offer these options whenever possible [22]. Ultimately, human relationships are central to growth and healing—and technology, when used thoughtfully, can be a powerful enabler of connection and support [58].
Aphasia, a language impairment resulting from brain injury, is a common consequence of stroke [62–64]. It ranges from complete loss of speech to fluent but error-filled language [62]. This condition often leads to social isolation, loneliness, frustration, and fatigue, compounded by other physical or sensory deficits [63], (see Table 5). Survivors may feel guilt or fear of being a burden to family and friends due to their reduced ability to communicate and provide support [63].
The language barrier and lack of targeted interventions contribute to the loss of social connections, especially early in recovery, reducing the quality and number of friendships [64]. This isolation impacts physical and mental health, increasing risks of depression, anxiety, mood swings, and chronic stress [63–66]. To manage emotional shifts, strategies like daily routines, cooking, exercise, journaling, creative activities, and games are effective [63].
Aphasia restricts social interaction and community participation, making the preservation of social networks a key intervention goal [64]. Strong social ties enhance engagement in daily life and promote well-being. Encouraging connections between people with and without Aphasia supports community integration and improved quality of life [64].
The literature recommends including survivors, family, and friends in structured, collaborative interventions to boost social cohesion and reduce isolation [64]. This includes forming support groups and promoting interdisciplinary care—involving speech therapists, psychologists, and other professionals—to ensure personalized, comprehensive treatment [63,66].
However, challenges remain. Speech-language pathologists recognize the need to address emotional issues but often lack access to psychological support and face limits within their professional roles [65]. This gap underscores the need for training and collaboration to improve psychosocial care. Holistic, interdisciplinary strategies, supported by strong health policies, can transform aphasia care—centered on restoring communication and rebuilding meaningful lives [10,65].
Personalized interventions are critical to reflect each survivor’s unique recovery path. The LUNA program [67] offers a remote, individualized approach focusing on personal narratives and combining therapies like story grammar, mapping therapy, and semantic feature analysis. It emphasizes both metalinguistic (language awareness) and metacognitive (self-reflection) skills and was delivered via Zoom during the pandemic, enhancing motivation and meaningful engagement.
Similarly, the communiCATE protocol [68] is a technology-based reading therapy for people with Aphasia. It has shown promise in delivering structured, tech-supported rehabilitation, supporting effective and accessible post-stroke language recovery.
A major challenge for stroke survivors with Aphasia is maintaining adherence to interventions. Technology, especially VR, has shown promise in improving engagement and treatment outcomes [40,62]. VR offers an immersive and enjoyable experience that increases motivation and supports consistent language practice while minimizing the fear and embarrassment often associated with communication failures in real-life settings [40,62]. It helps transfer acquired skills beyond the clinical context and is positively associated with both cognitive and physical rehabilitation outcomes [40].
Two notable VR programs illustrate this potential:
●
●
Both studies reported excellent program adherence, high interaction levels, and lasting improvements in communication [62] and cognitive functions [40]. Participants appreciated the intuitive, accessible interfaces and engaging environments, which fostered independence and motivation. However, [62] emphasized the need for more targeted VR interventions to improve communicative confidence and reduce social isolation.
Additionally, many individuals with Aphasia seek clarity about their prognosis, yet little is known about how they experience receiving such feedback [69]. Delivering clear, compassionate updates is essential, especially given the emotional distress and potential negative effects poor communication may cause. A reframed understanding of “normality” in Aphasia—defined not by the absence of limitations but by the capacity to adapt—is crucial. Thoughtful feedback can help survivors accept their condition, adjust emotionally, and engage more effectively in recovery [69].
This study aims to explore the impact of therapeutic groups on promoting social support and well-being among stroke survivors, with a focus on therapeutic writing mediated by mobile apps, such as WhatsApp. Post-stroke recovery involves not only physical and cognitive challenges but also emotional adaptation for survivors, families, and caregivers. To support this multifaceted process, innovative strategies—therapeutic groups, writing, and digital tools—are essential for fostering autonomy and quality of life [38].
Interdisciplinarity and Social SupportInterdisciplinary collaboration among physiotherapists, psychologists, doctors, and other professionals enhances rehabilitation outcomes and supports overwhelmed caregivers [10,37,65]. This approach promotes personalized care, continuous monitoring, and a more humanized process.
Support networks—particularly therapeutic groups like GAMs—offer emotional benefits and reduce social isolation [6,52,59]. Whether in-person or online, these spaces promote resilience, emotional expression, and peer bonding, supporting adherence to therapy and community reintegration [13,16,60]. For caregivers, these groups offer emotional support, validation, and tools for stress management [16,41].
In addition to their psychological benefits, these groups act as cost-effective complements to formal mental health care, bridging professionals, survivors, and families in accessible and continuous support systems [6,10,60].
Therapeutic WritingTherapeutic writing is an effective tool for emotional regulation, self-reflection, and adaptation to post-stroke changes [41,42,46]. Whether through handwritten diaries [13] or digital platforms [1], it helps individuals manage distress, track cognitive fatigue, and adjust routines to improve well-being [13,44].
Writing fosters communication with health professionals, revealing emotional challenges and guiding care adjustments. It also strengthens caregivers’ understanding and involvement by encouraging the use of writing tools and participation in support networks [10,41,52].
Technological InnovationDigital tools have become crucial in stroke rehabilitation, enabling remote care, cognitive stimulation, and communication. Programs like LUNA [67], EVA Park [62], and Reh@City [40] integrate emotional, physical, and cognitive rehabilitation in accessible, engaging formats.
Apps like WhatsApp have shown particular effectiveness in supporting emotional expression and ongoing communication, especially during the COVID-19 pandemic [10,22,59]. These tools help overcome geographic and physical barriers, enhancing inclusion and social support [38,60].
For successful rehabilitation, professionals must adopt a holistic, personalized, and tech-informed approach, especially for individuals with communication impairments like Aphasia. Training in mobile technologies and adapting care to survivors’ needs ensures digital inclusion and therapeutic adherence [40,65,67].
Caregivers also benefit from these platforms by accessing educational resources, peer support, and emotional relief [1,56,70], creating a network that fosters mutual understanding and continuous engagement.
While the combination of WhatsApp-mediated support and therapeutic writing for stroke survivors is promising, direct empirical evidence in this population remains limited. As a result, parts of the discussion draw on related contexts, such as palliative care, digital health interventions, and general social media use, to provide insights into potential mechanisms and effects.
We have explicitly indicated where evidence is extrapolated from these related contexts, to ensure transparency. These insights serve to highlight gaps in the literature and generate hypotheses for future research, rather than to provide definitive conclusions.
Despite these limitations, the findings suggest that digital interventions may enhance social support and well-being in stroke rehabilitation. The review underscores the need for high-quality studies directly investigating WhatsApp-mediated therapeutic writing in stroke populations, including rigorous outcome measurement, standardized interventions, and long-term follow-up.
By situating the current evidence within a broader context, this discussion both clarifies the novelty of the approach and provides actionable guidance for future research efforts.
LimitationsThis systematic review has several limitations that should be considered when interpreting the findings. First, there is notable heterogeneity among the included studies, including differences in interventions (e.g., therapeutic writing, group therapy, digital platforms), outcome measures (various definitions and scales for social support and well-being), and study designs. This variability may limit the comparability of studies and the generalizability of conclusions.
Second, the review relied on a limited number of databases (B-on, PubMed, Google Scholar, and Google), which may have resulted in the omission of some relevant studies. While additional complementary studies were identified through manual searches, this process cannot entirely eliminate potential selection bias.
Third, although efforts were made to minimize subjectivity by employing independent reviewers for study selection and data extraction, some degree of subjectivity in decisions on eligibility and interpretation of results is unavoidable.
Fourth, while a systematic risk of bias assessment has been conducted using appropriate tools (Cochrane RoB, RoBANS, and CASP for qualitative studies), variability in study quality and reporting completeness may affect the reliability of some findings.
Finally, the narrative synthesis approach, used due to heterogeneity of interventions and outcomes, inherently limits the ability to conduct quantitative comparisons or meta-analysis.
Despite these limitations, the review provides a transparent and comprehensive overview of the current evidence and highlights key gaps and trends for future research.
Also the number of eligible studies identified through systematic screening was relatively small, which restricts the breadth of evidence available for synthesis. To provide a more comprehensive perspective, we incorporated additional sources narratively; however, these complementary studies do not hold the same evidential weight as those identified systematically and should be interpreted with caution. Second, the included studies vary considerably in methodology, sample characteristics, and outcome measures, which introduces heterogeneity and limits the comparability of results across studies. Finally, while efforts were made to minimize bias through systematic screening and quality appraisal, the reliance on heterogeneous and, in some cases, emerging evidence inevitably affects the generalizability of the conclusions. These limitations highlight the need for further high-quality, methodologically consistent research in this area.
In summary, the evidence reviewed supports the role of therapeutic writing and digital communication tools, particularly WhatsApp, as potential facilitators of psychological well-being. These findings are grounded in the systematically identified studies and provide an emerging but promising evidence base. Beyond these evidence-based insights, we also propose broader recommendations for clinical practice and future research, recognizing that such extrapolations extend beyond the available data. These recommendations should therefore be considered as informed reflections rather than definitive conclusions, underscoring the importance of further empirical work to consolidate this field.
Based on the gaps identified in the current literature, several recommendations for future research can be made. First, there is a need for high-quality RCTs to evaluate the effectiveness of WhatsApp and other digital interventions in stroke rehabilitation, with clearly defined outcomes such as social support, well-being, and functional recovery.
Second, studies should include larger and more diverse populations, considering variables such as age, stroke severity, and socio-cultural context, to improve the generalizability of findings.
Third, the use of standardized and validated outcome measures is recommended to enable comparison across studies and strengthen evidence synthesis.
Fourth, future studies should consider long-term follow-up to assess the sustainability of intervention effects over time.
Finally, investigating the mechanisms of action through which digital interventions influence social support, engagement, and rehabilitation adherence—including qualitative research to capture patient experiences—would provide valuable insights into how these interventions work in practice.
Implementing these recommendations will help address the current scarcity of robust evidence and guide the development of effective, evidence-based digital interventions in stroke rehabilitation.
However, digital technologies, when combined with therapeutic practice, not only strengthen physical and cognitive rehabilitation but also enhance survivors' emotional well-being, promoting a humanized care. This combination of social support, personalized interventions and conscious use of technology can transform challenges into opportunities for growth and emotional strengthening, promoting comprehensive and humane care.
Not applicable.
Declaration of Helsinki STROBE Reporting GuidelineThis study adhered to the Helsinki Declaration. The Strengthening the Reporting of Observational studies in Epidemiology (STROBE) reporting guideline was followed.
No data were generated from the study.
Conceptualization, IdSS and LS; Methodology, MR; Software, MR; Validation, IdSS and LS; Formal Analysis, MR; Investigation, MR; Resources, MR; Data Curation, IdSS and LS; Writing—Original Draft Preparation, MR; Writing—Review & Editing, IdSS and LS; Visualization, MR; Supervision, IdSS and LS; Project Administration, IdSS and LS.
The authors declares that they have no conflicts of interest.
Bebiana Silva, Junior Clinical Psychologist and one of the judges of the narratives.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
Rodrigue M, Santos Silva Id, Soares L. Connections that care: WhatsApp as a support space for stroke survivors. Adv Geriatr Med Res. 2025;7(3):e250020. https://doi.org/10.20900/agmr20250020.

Copyright © Hapres Co., Ltd. Privacy Policy | Terms and Conditions